The Centre of Research Excellence on Meaningful Outcomes in Substance Use Treatment’s mission is to reduce the cost and burden of primary and comorbid alcohol and other drug (AOD) problems in Australia, by increasing the AOD sector’s capacity to deliver evidence-based and cost-effective care.
To achieve this, a Value-Based model of Healthcare (VBHC) will be developed, which shifts the focus away from the volume of service delivery toward improving client outcomes (value) through the delivery of the best quality and most cost-effective AOD treatment available.
Routine outcome measures and feedback (ROMF) are at the cornerstone of VBHC, which aims to:
- Identify what outcomes matter to clients.
- Identify and implement a standard set of Routine Outcome Measures (ROM) to assess, monitor and provide individual feedback on treatment progress (ROMF); and
- Identify which service types or settings provide the best outcomes for different types of AOD presentations.
Restructuring care delivery around client outcomes through ROMF, has been found to improve the quality and cost effectiveness of healthcare for a range of physical (e.g., pain, general health) and mental health (depression, anxiety) conditions. ROMF also increases access to healthcare by curbing inefficiencies, streamlining clinical decision making, and delivering the right care in the right setting at the right time. There is accumulating evidence that ROMF has positive effects in AOD treatment settings on client treatment adherence, completion, and outcomes. However, despite this evidence and decades of calls for AOD services to undertake ROMF, few attempts have been made to implement them, due to the challenges involved including; the lack of consensus agreement on AOD outcome measures and how to best implement them; limited uptake of ROMF; and numerous other individual (client and staff), systems and organizational barriers.
This Centre of Research Excellence (CRE) will develop a new model of Value-Based AOD Healthcare by conducting a series of research projects addressing the three pillars of VBHC: Quality Improvement, Informed Decision Making, and Cost Effectiveness.
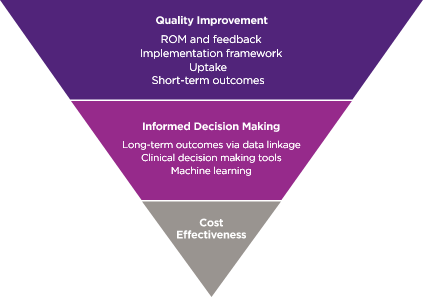
Quality improvement will be achieved through the implementation of a standard set of ROM measures into clinical care to assess and track client outcomes over time. The resulting data is then used to inform decision making by defining thresholds or benchmarks for clinically significant change on key outcome variables. Predictive models using machine learning will also be used to inform clinical decision making. Data linkage will generate new knowledge about the outcomes and cost-effectiveness of different types of AOD services and point-in-time indicators, identifying which clients presenting with different drugs of concern/polydrug use/comorbid mental health problems are most likely to respond to treatment types/settings at different time points.
Specifically, our research aims to:
- Determine the most effective way to maximize the uptake of routine outcome measures and feedback among AOD services, clients, and staff.
- Examine the impact of ROMF on:
- Client AOD treatment adherence and outcomes.
- AOD service access, efficiency, and cost-effectiveness.
- Staff satisfaction, burnout, and turnover.
- Examine the short- and long-term client outcomes of different AOD service types and settings using ROMF and data linkage.
- Identify which AOD service types and settings have the best outcomes and are most cost effective for different types of AOD, polydrug use and comorbid mental health presentations using machine learning.
